Dental sterilization is paramount in dentistry. Most dentists’ offices share a familiar vibe, one we can only describe as “sterile.” Dentists follow strict cleanliness rules to prevent infections and diseases. As practices begin to reopen for the first time since the COVID-19 pandemic hit, dentists are stepping up sterilization protocols to ensure that your next visit will be a safe one.
Toronto dentist Dr. Jeanie Luong says dentists need to communicate with staff and patients at every step. For patients who are nervous about coming in, “We assure them that we take the health and safety of our patients and staff very seriously and that we have taken every precaution to ensure they have a safe visit,” she says.
When it comes to regular sterilization practices, staff training, and enhanced measures, dentists do a few things to keep their offices clean and sterile.
Dental sterilization protocol
Laws and regulations for dental practices vary across Canada, but every province and territory has a regulatory body (called a college) that licenses dentists and sets health and safety standards. Provincial colleges align their standards with local public health units and the Provincial Infectious Diseases Advisory Committee on Infection Prevention and Control (PIDAC-IPC).
It’s a mouthful of an acronym, but PIDAC-IPC publishes best practices, recommendations and self-assessment checklists intending to prevent disease transmission in clinical offices. These practices and procedures are known as infection prevention and control or IPAC.
Dr. Luong says guidelines for dentists are “detailed, technical and rigorous.” Staff training isn’t just a one-time deal, either—ongoing education, training and support are necessary to help staff work safely. Dr. Luong says IPAC manuals should be available in the office for staff to review regularly.
How to sterilize dental equipment
Dentists use both single-use and reusable instruments to complete dental work. Cleaning dental equipment requires a sterilization area—every office has one, and it looks a bit like an office kitchen.
Sterilization areas are designed to prevent cross-contamination. There are designated areas for receiving instruments, cleaning and decontamination, drying, packaging, sterilization and storage. It’s an efficient one-way workflow (dirty to clean.)
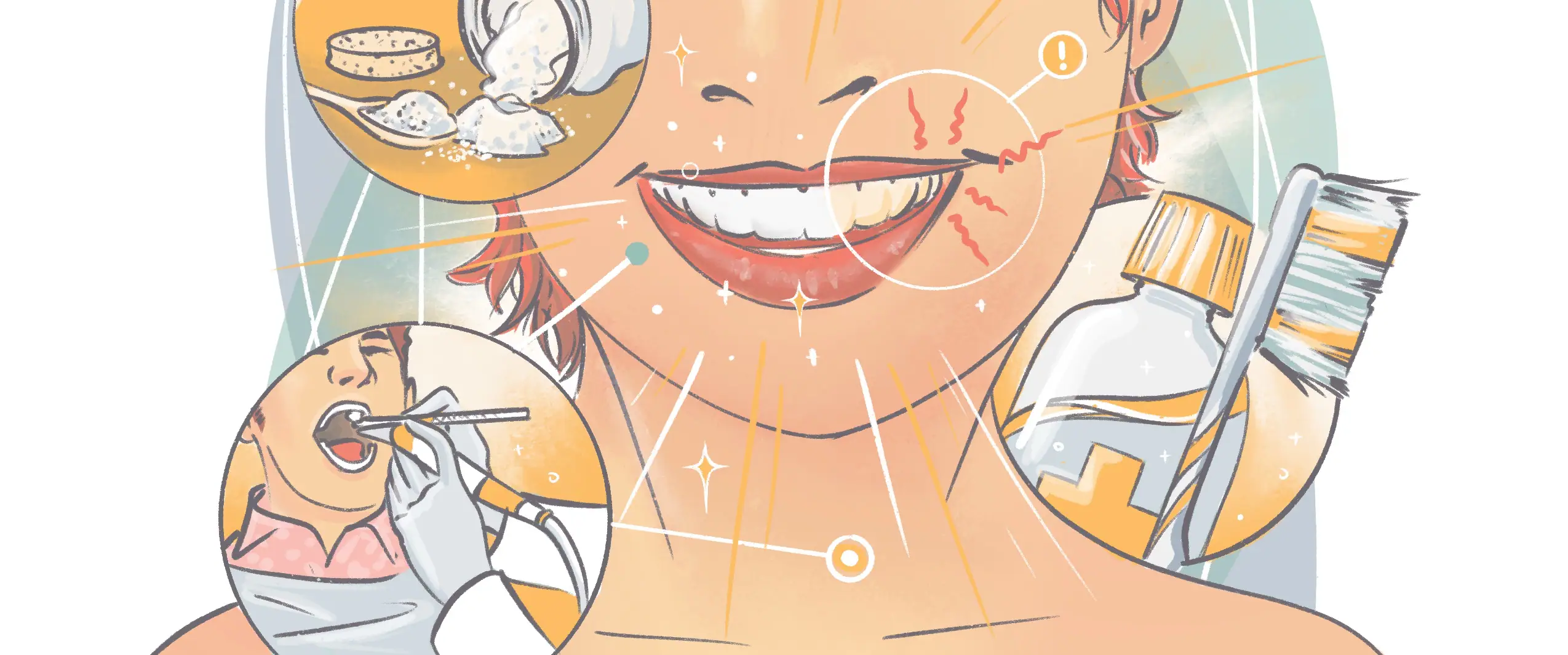
Here’s a step-by-step process of how to sterilize dental instruments:
- Clean and decontaminate: The dirty instruments are brought into the sterilization area in a sealed container, scrubbed, and placed in an ultrasonic cleaner, which is a container filled with a disinfectant solution that vibrates to remove any remaining debris.
- Package: The instruments are wrapped in kits or sealed packages, stamped with a date, cycle, and user ID sticker (for tracking and quality control).
- Sterilize: After the instruments are packaged, the sterilization process involves putting the instruments in an autoclave, which uses steam pressure and high heat for a sustained period, which inactivates all bacteria and viruses.
- Test: Indicator stripes are placed into the pouches to confirm that the equipment inside achieves adequate temperature and pressure. When the process is complete, the strip changes colour. After that, a spore test makes sure no bacteria survived.
- Storage: Once the cleaning and sterilization cycle is complete, the packaged clean instruments are stored in an enclosed area on the room’s designated “clean side.” The instruments are only retrieved and unwrapped once a patient is in the chair.
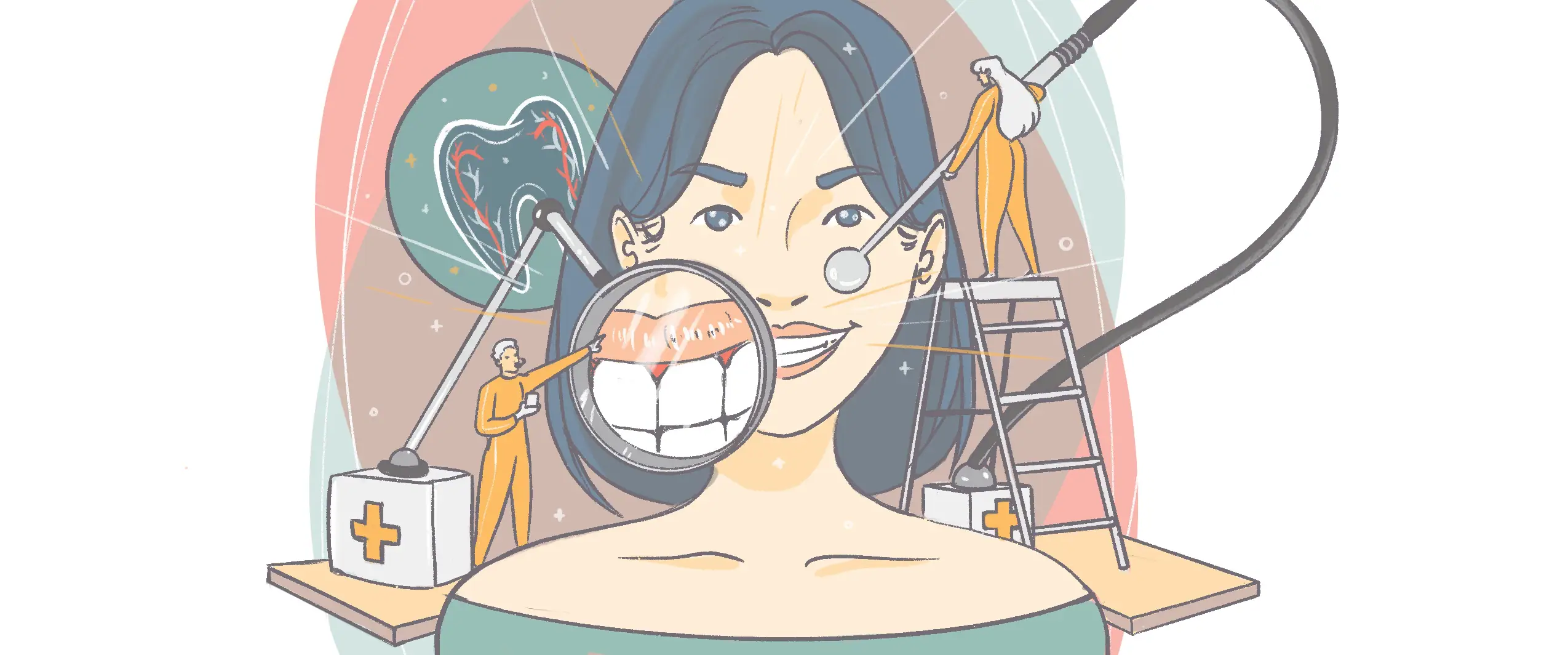
Enhanced safety measures after COVID-19
When your dentist’s office is ready to reopen, you’ll likely receive a call, email or text outlining new policies and precautions for appointments. Every dentist’s office will be different, but here are a few general things you can expect:
- Pre-screening and temperature taking.
- Masks and hand sanitizer for the reception area/waiting room.
- Staggered appointment. This allows for minimal contact between patients and extra time for enhanced cleaning and disinfection procedures.
- Enhanced personal protective equipment (PPE) for staff.
- Rinsing with a hydrogen peroxide solution before your appointment.
Dr. Luong’s dental practice created an illustrated and easy-to-read infographic to communicate enhanced safety precautions and is emailing it to patients, to give them a heads up on her office’s new procedures. Some dentists may accommodate special requests for nervous patients, such as booking the first or last appointment of the day.
“We understand if [patients] are still uncomfortable and not ready to come in, so we assure them that we are here for them whenever they are ready,” Dr. Luong says.
Communicating is key
During uncertain times, ongoing communication between dentists, staff and patients is important. For dentists, it boils down to being proactive by creating protocols and procedures, training staff, communicating with patients before a visit, and reinforcing the message through actions once patients arrive. Dr. Luong has posted their new precautions in every treatment room to encourage engagement with patients.
“People need to know what you are doing; it isn’t enough to do it quietly without sharing your message.”